ご利用について
This PDQ cancer information summary has current information about the causes and treatment of lymphedema. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Date Last Modified") is the date of the most recent change. The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Supportive and Palliative Care Editorial Board.
CONTENTS
- What is lymphedema?
-
Lymphedema is swelling caused by a buildup of lymph fluid in the body between the skin and muscle. Lymph fluid is part of the lymph system, which plays a role in your body’s ability to fight infection and disease. If you have cancer, the cancer or cancer treatment can disrupt the flow of lymph fluid and cause lymphedema (also known as secondary lymphedema). Lymphedema may arise soon after cancer treatment, or it may develop years after treatment has ended. Most often, it develops slowly over months or years.
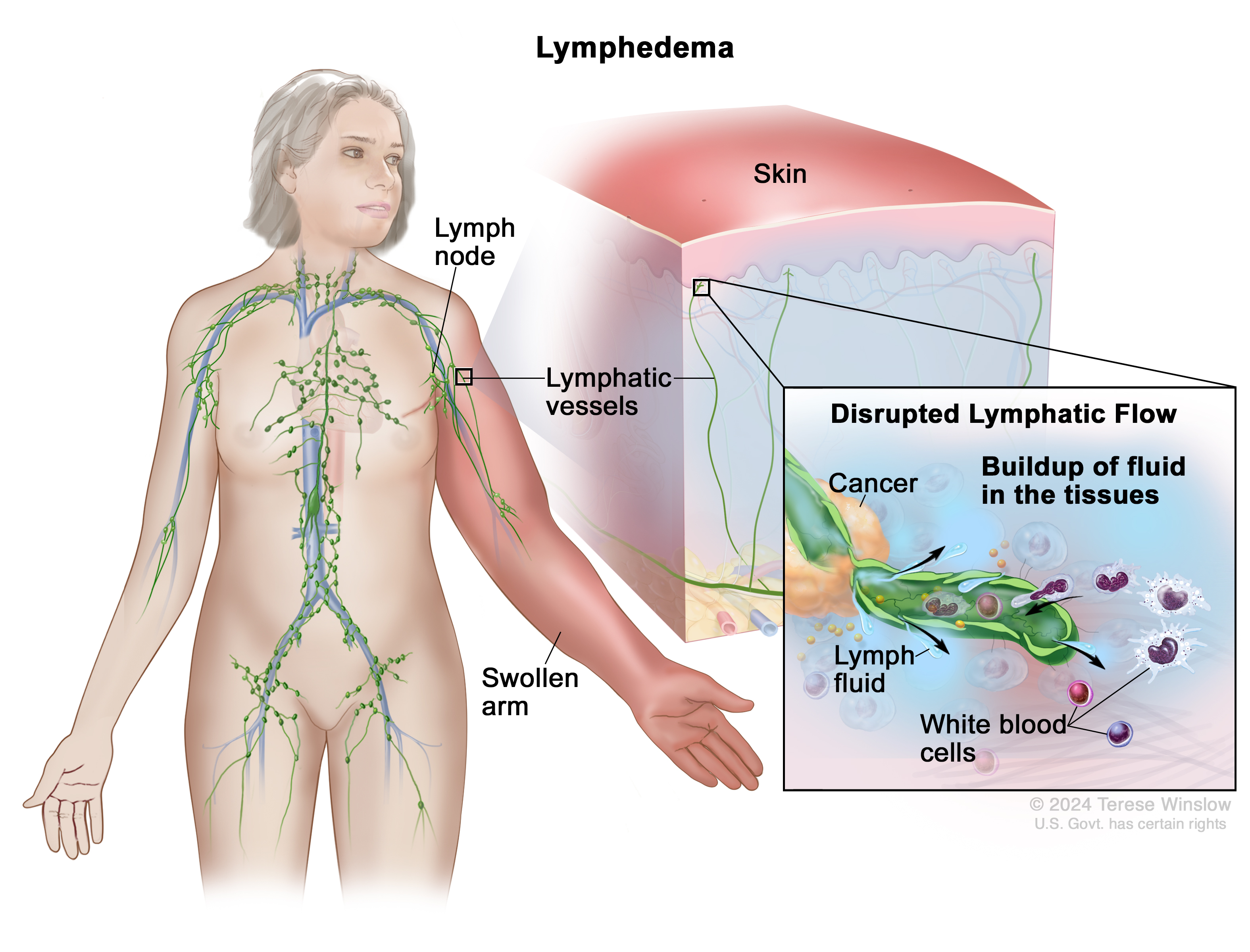
The lymph system helps the body fight infection and is made up of lymph nodes, lymphatic vessels, and organs that collect and carry lymph fluid through the body. If cancer or cancer treatment disrupts the flow of lymph fluid or damages lymph nodes and vessels, lymph fluid may build up and cause lymphedema. Although lymphedema cannot be prevented, there are ways to lower your risk or keep lymphedema from getting worse.
Once lymphedema develops, it is a chronic condition that cannot be cured but can be treated to relieve swelling and improve your ability to function day to day. Lymphedema is easier to control when treatment starts early, so contact your doctor as soon as you notice heaviness, swelling, or other signs of lymphedema.
What causes lymphedema?
Anything that blocks or changes the flow of lymph fluid in the body can cause lymphedema. Cancer and cancer treatments can cause lymphedema when:
Your risk for lymphedema depends on the type and location of your cancer and the treatments you have. Other risk factors for lymphedema include having an infection, healing slowly after surgery, having lymph nodes removed, past surgeries or radiation, having advanced cancer, and being overweight or having obesity. Talk with your doctor to learn about your risk of lymphedema.
Lymphedema and breast cancer
Treatment for breast cancer often involves surgery that removes one or more lymph nodes in the underarm area, increasing the risk of lymphedema. If you have been treated for breast cancer with radiation therapy or surgery, you may develop lymphedema in your hand, arm, or chest on the side of the body where lymph nodes were removed or damaged.
Lymphedema and other cancers
Lymphedema can occur anywhere in the body, but it most commonly affects an arm or leg. Some cancers—especially those that form in the abdomen or genital area—and their treatments are more likely than others to cause lymphedema because they are located near lymph nodes and vessels. Lymphoma, a cancer that affects white blood cells (part of the lymph system), can also cause lymphedema as white blood cells build up and block lymph flow.
The type of cancer you have can help predict where you may develop lymphedema.
Lymphedema can also develop after surgery for melanoma and sarcoma.
What are symptoms of lymphedema?
You may notice symptoms of lymphedema in an arm or leg or near where you had surgery or received radiation therapy. Signs and symptoms may develop slowly over time, so pay close attention to any slight changes. Contact your doctor if you notice any of these signs of lymphedema.
Signs and symptoms of lymphedema anywhere in the body
Signs and symptoms of lymphedema in the arms or legs
Lymphedema in your arm or leg may cause these additional signs and symptoms:
Signs and symptoms of lymphedema in the head or neck
Lymphedema in your head or neck may cause these additional signs and symptoms:
Signs and symptoms of lymphedema in the genitals or abdomen
Lymphedema in your genitals or abdomen may cause these additional signs and symptoms:
Lymphedema and cellulitis
Cellulitis is a potentially life-threatening bacterial infection of the skin that is a common complication of lymphedema. People with lymphedema are at greater risk of cellulitis because skin in swollen areas is stretched thin, allowing easier entry of bacteria that thrive in fluid-rich areas of the body.
Some signs and symptoms of cellulitis are similar to those of lymphedema. Always check with your doctor about any skin changes or other symptoms you experience. Symptoms of cellulitis include:
If you have a fever or other signs of cellulitis, call your doctor right away. If left untreated, cellulitis can become life-threatening. Your doctor can prescribe antibiotics to treat cellulitis.
How is lymphedema diagnosed?
You should watch for lymphedema signs and symptoms, such as tightness or swelling in an arm or leg, during and after cancer treatment. If you alert your doctor to swelling or other changes you have noticed, your doctor will examine the swollen part of your body. If swelling is affecting an arm or leg, they will compare the size of your swollen arm or leg with that of the other limb.
You may also have one or more of the following tests to help your doctor better understand the cause of swelling and what is disrupting the flow of lymph fluid:
Lymphedema stages
If you are diagnosed with lymphedema, your doctor will use a staging system to describe the severity of your lymphedema.
How is lymphedema treated?
Treatments are available for managing the symptoms of lymphedema. Your health care team will talk with you about management techniques that can be done at home or under the supervision of a trained professional such as a nurse or a certified lymphedema therapist (CLT), a physical or occupational therapist trained to treat lymphedema. Treatments include:
Short stretch bandaging, compression wraps, leggings, or stockings
These can help move fluid around in your arms and legs to prevent it from building up. They may also be called compression garments. Your nurse or CLT will help you find garments that fit properly and will show you how to use them.
Manual lymphatic drainage
Manual lymphatic drainage, also called lymphatic drainage massage, involves gentle massage that helps move lymph fluid through the body. Lymphatic drainage is part of a treatment called complete decongestive therapy, which is managed by a CLT. Complete decongestive therapy may also include bandaging, exercises, and skin care to manage symptoms.
Compression pump
This is a device connected to a compression sleeve or sock that applies pressure intermittently to the arm or leg. The pumping action may help keep lymph fluid moving, preventing buildup in the limbs.
Surgery and other treatments
If lymphedema is advanced, your doctor may recommend surgery or another medical treatment.
Can I prevent lymphedema?
Although there is no way to prevent lymphedema, there are things you can do to lower your risk or keep it from getting worse. Your health care team may suggest the following things you can do at home:
Talking with your doctor about lymphedema
As you prepare for a visit with your doctor, nurse, or social worker, consider making a list of questions to ask and adding these questions about lymphedema:
Coping with lymphedema
The physical changes that result from lymphedema can affect your well-being. You may not be able to do the activities you once enjoyed or find clothes that fit properly. You may feel uncomfortable with the way you look and isolated from those around you. Working with a CLT is often the best way to manage and cope with lymphedema.
Side effects like lymphedema can be hard to deal with, both physically and emotionally. It’s important to ask for support from your health care team. They can help you prepare for and make it through difficult times. Learn more about ways to cope with cancer including emotions that people with cancer often have and ways to adjust to daily life during cancer treatment.
For family members and friends who are caring for someone with cancer, you may find these suggestions for caregivers to be helpful.
Lymphedema research
Research is ongoing to discover new ways to prevent, diagnose, and treat lymphedema. Research studies called clinical trials help advance knowledge about lymphedema and other side effects of cancer and cancer treatment. Learn more at Clinical Trials Information for Patients and Caregivers.
To find NCI-supported clinical trials for lymphedema, go to Lymphedema Clinical Trials. Clinical trials supported by other organizations can be found at ClinicalTrials.gov.
Advances in cancer surgery and treatments are helping reduce the chances of lymphedema in people with cancer. For example, sentinel lymph node biopsy allows doctors to remove fewer lymph nodes when checking if the cancer has spread, decreasing the risk of lymphedema.
Related Resources

 画像を拡大する
画像を拡大する