ご利用について
This PDQ cancer information summary has current information about the treatment of childhood liver cancer. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Date Last Modified") is the date of the most recent change. The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Pediatric Treatment Editorial Board.
CONTENTS
- Hepatoblastoma
-
Hepatoblastoma is a disease in which malignant (cancer) cells form in the tissues of the liver. It is the most common type of childhood liver cancer and usually affects children younger than 3 years of age.
The liver is one of the largest organs in the body. It has two lobes and fills the upper right side of the abdomen inside the rib cage. Three of the many important functions of the liver are the following:
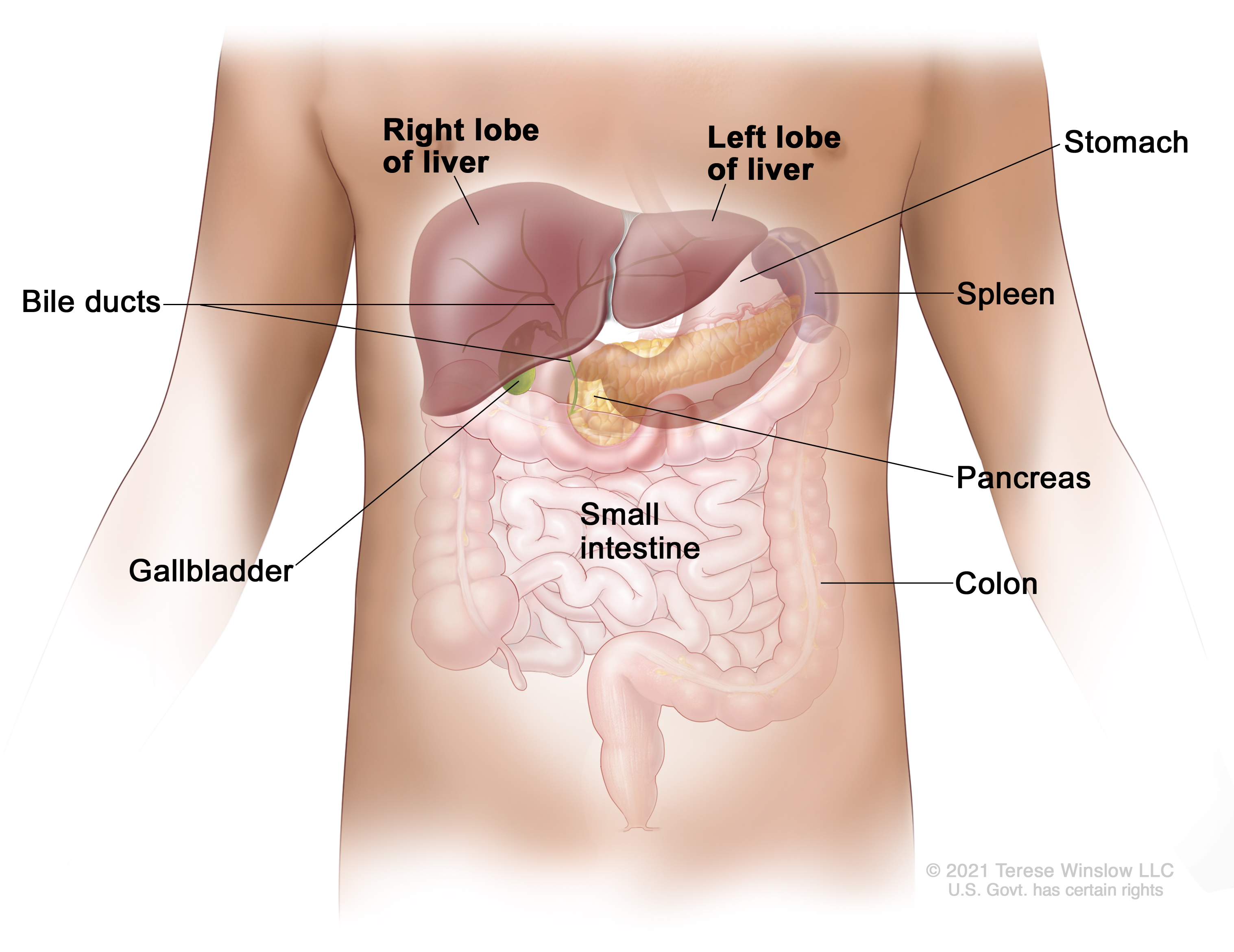
Anatomy of the liver. The liver is in the upper abdomen near the stomach, intestines, gallbladder, and pancreas. The liver has a right lobe and a left lobe. Each lobe is divided into two sections (not shown). In hepatoblastoma, the histology (how the cancer cells look under a microscope) affects the way the cancer is treated. The histology for hepatoblastoma may be one of the following:
Signs and symptoms of hepatoblastoma
Signs and symptoms are more common after the tumor gets big. Other conditions can cause the same signs and symptoms. Check with your child’s doctor if your child has any of the following:
Causes and risk factors for hepatoblastoma
Anything that increases your chance of getting a disease is called a risk factor. Not every child with one or more of these risk factors will develop hepatoblastoma, and hepatoblastoma will develop in some children who don’t have any known risk factors. Talk with your child’s doctor if you think your child may be at risk.
The following syndromes or conditions are risk factors for hepatoblastoma:
Children at risk of developing hepatoblastoma may have tests done to check for cancer before any symptoms appear. Every 3 months until the child is 4 years old, an abdominal ultrasound exam is done and the level of alpha-fetoprotein in the blood is checked.
Diagnosis of hepatoblastoma
Tests that examine the liver and the blood are used to diagnose hepatoblastoma and find out whether the cancer has spread.
The following tests and procedures may be used:
Prognostic factors for hepatoblastoma
The prognosis(chance of recovery) and treatment options for hepatoblastoma depend on the following:
- the PRETEXT group
- the size of the tumor
- whether the type of hepatoblastoma is well-differentiated fetal (pure fetal) or small cell undifferentiated histology
- whether the cancer has spread to other places in the body, such as the diaphragm, lungs, or certain large blood vessels
- whether there is more than one tumor in the liver
- whether the outer covering around the tumor has broken open
- how the cancer responds to chemotherapy
- whether the cancer can be removed completely by surgery
- whether the patient can have a liver transplant
- whether the AFP blood levels go down after treatment
- the age of the child
- whether the cancer has just been diagnosed or has recurred
For hepatoblastoma that recurs (comes back) after initial treatment, the prognosis and treatment options depend on the following:
- where in the body the tumor recurred
- the type of treatment used to treat the initial cancer
Hepatoblastoma may be cured if the tumor is small and can be completely removed by surgery.
Stages of hepatoblastoma
After hepatoblastoma has been diagnosed, tests are done to find out if cancer cells have spread within the liver or to other parts of the body. The process used to find out if cancer has spread within the liver, to nearby tissues or organs, or to other parts of the body is called staging.In hepatoblastoma, the PRETEXT and POSTTEXT groups are used instead of stage to plan treatment. The results of the tests and procedures done to detect, diagnose, and find out whether the cancer has spread are used to determine the PRETEXT and POSTTEXT groups.
Two grouping systems are used for hepatoblastoma to decide whether the tumor can be removed by surgery:
- The PRETEXT group describes the tumor before the patient has any treatment.
- The POSTTEXT group describes the tumor after the patient has had treatment such as neoadjuvant chemotherapy.
The liver is divided into four sections. The PRETEXT and POSTTEXT groups depend on which sections of the liver have cancer. There are four PRETEXT and POSTTEXT groups.
PRETEXT and POSTTEXT group I

Liver PRETEXT and POSTTEXT I. Cancer is found in one section of the liver. Three sections of the liver that are next to each other do not have cancer in them. In group I, the cancer is found in one section of the liver. Three sections of the liver that are next to each other do not have cancer in them.
PRETEXT and POSTTEXT group II

Liver PRETEXT and POSTTEXT II. Cancer is found in one or two sections of the liver. Two sections of the liver that are next to each other do not have cancer in them. In group II, cancer is found in one or two sections of the liver. Two sections of the liver that are next to each other do not have cancer in them.
PRETEXT and POSTTEXT group III

Liver PRETEXT and POSTTEXT III. Cancer is found in three sections of the liver and one section does not have cancer in it, or cancer is found in two sections of the liver and two sections that are not next to each other do not have cancer in them. In group III, one of the following is true:
- Cancer is found in three sections of the liver and one section does not have cancer.
- Cancer is found in two sections of the liver and two sections that are not next to each other do not have cancer in them.
PRETEXT and POSTTEXT group IV

Liver PRETEXT and POSTTEXT IV. Cancer is found in all four sections of the liver. In group IV, cancer is found in all four sections of the liver.
Sometimes hepatoblastoma continues to grow or comes back after treatment.
Progressive disease is cancer that continues to grow, spread, or worsen. Progressive disease may be a sign that the cancer has become refractory to treatment.
Recurrent hepatoblastoma is cancer that has recurred (come back) after it has been treated. The cancer may come back in the liver or in other parts of the body. To learn more about metastatic cancer (cancer that has spread from where it started to other parts of the body), see Metastatic Cancer: When Cancer Spreads.
Types of treatment for hepatoblastoma
Children with hepatoblastoma should have their treatment planned by a team of healthcare providers who are experts in treating this rare childhood cancer. Treatment will be overseen by a pediatric oncologist, a doctor who specializes in treating children with cancer. The pediatric oncologist works with other healthcare providers who are experts in treating children with hepatoblastoma and who specialize in certain areas of medicine. It is especially important to have a pediatric surgeon with experience in liver surgery who can send patients to a liver transplant program if needed. Other specialists may include the following:
- pediatrician
- radiation oncologist
- pediatric nurse specialist
- rehabilitation specialist
- psychologist
- social worker
- nutritionist
For more information about having a child with cancer and ways to cope and find support, see Childhood Cancers.
Every child will not receive all the treatments listed below. Your child’s care team will help you make treatment decisions based on your child’s unique situation. To learn more about factors that help determine the treatment plan for hepatoblastoma, see Prognostic factors for hepatoblastoma.
Surgery
When possible, the cancer is removed by surgery. The types of surgery that may be done are:
- Partial hepatectomy: The part of the liver where cancer is found is removed by surgery. The part removed may be a wedge of tissue, an entire lobe, or a larger part of the liver, along with a small amount of normal tissue around it.
- Total hepatectomy and liver transplant: The entire liver is removed by surgery, followed by a transplant of a healthy liver from a donor. A liver transplant may be possible when cancer has not spread beyond the liver and a donated liver can be found. If the patient has to wait for a donated liver, other treatment is given as needed.
- Resection of metastases: Surgery is done to remove cancer that has spread outside of the liver, such as to nearby tissues, the lungs, or the brain.
The type of surgery that can be done depends on the following:
- the PRETEXT group and POSTTEXT group
- the size of the primary tumor
- whether there is more than one tumor in the liver
- whether the cancer has spread to nearby large blood vessels
- the level of AFP in the blood
- whether the tumor can be shrunk by chemotherapy so that it can be removed by surgery
- whether a liver transplant is needed
Chemotherapy is sometimes given before surgery to shrink the tumor and make it easier to remove. This is called neoadjuvant therapy.
After the doctor removes all the cancer that can be seen at the time of the surgery, some patients may be given chemotherapy or radiation therapy after surgery to kill any cancer cells that are left. Treatment given after the surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
Watchful waiting
Watchful waiting is closely monitoring a patient’s condition without giving any treatment until signs or symptoms appear or change. In hepatoblastoma, this treatment is only used for small tumors that have been completely removed by surgery.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy). Treatment using more than one anticancer drug is called combination chemotherapy.
Chemoembolization of the hepatic artery (the main artery that supplies blood to the liver) is a type of regional chemotherapy used to treat childhood liver cancer that cannot be removed by surgery. The anticancer drug is injected into the hepatic artery through a catheter (thin tube). The drug is mixed with a substance that blocks the artery, cutting off blood flow to the tumor. Most of the anticancer drug is trapped near the tumor and only a small amount of the drug reaches other parts of the body. The blockage may be temporary or permanent, depending on the substance used to block the artery. The tumor is prevented from getting the oxygen and nutrients it needs to grow. The liver continues to receive blood from the hepatic portal vein, which carries blood from the stomach and intestine to the liver. This procedure is also called transarterial chemoembolization or TACE.
The way the chemotherapy is given depends on the type of the cancer being treated and the PRETEXT or POSTTEXT group.
To learn more about chemotherapy and its side effects, see Chemotherapy and You: Support for People with Cancer.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. The way the radiation therapy is given depends on the type of the cancer being treated and the PRETEXT or POSTTEXT group.
There are two types of radiation therapy:
- External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer. External radiation therapy is used to treat hepatoblastoma that cannot be removed by surgery or has spread to other parts of the body.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
Radioembolization is a type of internal radiation therapy used to treat hepatoblastoma. A very small amount of a radioactive substance is attached to tiny beads that are injected into the hepatic artery (the main artery that supplies blood to the liver) through a thin tube called a catheter. The beads are mixed with a substance that blocks the artery, cutting off blood flow to the tumor. Most of the radiation is trapped near the tumor to kill the cancer cells. This is done to relieve symptoms and improve quality of life for children with hepatoblastoma.
To learn more about radiation therapy and its side effects, see Radiation Therapy to Treat Cancer and Radiation Therapy Side Effects.
Ablation therapy
Ablation therapy removes or destroys tissue. Different types of ablation therapy are used for liver cancer:
- Radiofrequency ablation: Special needles are inserted directly through the skin or through an incision in the abdomen to reach the tumor. High-energy radio waves heat the needles and tumor which kills cancer cells. Radiofrequency ablation is being used to treat recurrent hepatoblastoma.
- Percutaneous ethanol injection: A small needle is used to inject ethanol (pure alcohol) directly into a tumor to kill cancer cells. Treatment may require several injections. Percutaneous ethanol injection is being used to treat recurrent hepatoblastoma.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells. Targeted therapies usually cause less harm to normal cells than chemotherapy or radiation therapy do. Targeted therapy is being studied for the treatment of hepatoblastoma that has come back after treatment.
To learn more about how targeted therapy works against cancer, what to expect when having targeted therapy, and targeted therapy side effects, see Targeted Therapy to Treat Cancer.
Clinical trials
A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. For some patients, taking part in a clinical trial may be an option.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
To learn more about clinical trials, see Clinical Trials Information for Patients and Caregivers.
Long-term side effects of treatment
Side effects from cancer treatment that begin after treatment and continue for months or years are called long-term or late effects. Late effects of cancer treatment may include the following:
- physical problems
- changes in mood, feelings, thinking, learning, or memory
- second cancers (new types of cancer)
Some late effects may be treated or controlled. It is important to talk with your child's doctors about the long-term effects cancer treatment can have on your child. For more information, see Late Effects of Treatment for Childhood Cancer.
Follow-up tests
Some of the tests that were done to diagnose the cancer or to find out the treatment group may be repeated. Some tests will be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Treatment of newly diagnosed hepatoblastoma
Treatment options for newly diagnosed hepatoblastoma that can be removed by surgery at the time of diagnosis may include the following:
- surgery to remove the tumor, followed by combination chemotherapy for hepatoblastoma that is not well-differentiated fetal histology or aggressive chemotherapy for small cell undifferentiated histology
- surgery to remove the tumor, followed by watchful waiting or chemotherapy, for hepatoblastoma with well-differentiated fetal histology
Treatment options for newly diagnosed hepatoblastoma that cannot be removed by surgery or is not removed at the time of diagnosis may include the following:
- combination chemotherapy to shrink the tumor, followed by surgery to remove the tumor
- combination chemotherapy, followed by a liver transplant
- chemoembolization of the hepatic artery to shrink the tumor, followed by surgery to remove the tumor
- if the tumor in the liver cannot be removed by surgery but there are no signs of cancer in other parts of the body, the treatment may be a liver transplant
For newly diagnosed hepatoblastoma that has spread to other parts of the body at the time of diagnosis, combination chemotherapy is given to shrink the tumors in the liver and cancer that has spread to other parts of the body. After chemotherapy, imaging tests are done to check whether the tumors can be removed by surgery.
Treatment options may include the following:
- If the tumor in the liver and other parts of the body (usually nodules in the lung) can be removed, surgery will be done to remove the tumors followed by chemotherapy to kill any cancer cells that may remain.
- If the tumor in other parts of the body cannot be removed or a liver transplant is not possible, chemotherapy, chemoembolization of the hepatic artery, or radiation therapy may be given.
- If the tumor in other parts of the body cannot be removed or the patient does not want surgery, radiofrequency ablation may be given.
Treatment options in clinical trials for newly diagnosed hepatoblastoma include the following:
- a clinical trial of chemotherapy and surgery
Treatment of progressive or recurrent hepatoblastoma
Treatment of progressive or recurrent hepatoblastoma may include the following:
- surgery to remove isolated (single and separate) metastatic tumors with or without chemotherapy
- radiofrequency ablation
- combination chemotherapy
- liver transplant
- ablation therapy (radiofrequency ablation or percutaneous ethanol injection) as palliative therapy to relieve symptoms and improve the quality of life
- a clinical trial that checks a sample of the patient's tumor for certain gene changes to determine the type of targeted therapy that will be given to the patient
- Childhood Hepatocellular Carcinoma
-
Childhood hepatocellular carcinoma is a rare type of cancer that forms in liver cells called hepatocytes. Hepatocytes are the most common cells of the liver, and they carry out most of the functions of the liver.
The liver is one of the largest organs in the body. It has two lobes and fills the upper right side of the abdomen inside the rib cage. Three of the many important functions of the liver are the following:
- to make bile to help digest fats from food
- to store glycogen (sugar), which the body uses for energy
- to filter harmful substances from the blood so they can be passed from the body in stools and urine
Anatomy of the liver. The liver is in the upper abdomen near the stomach, intestines, gallbladder, and pancreas. The liver has a right lobe and a left lobe. Each lobe is divided into two sections (not shown). Childhood hepatocellular carcinoma usually affects older children and adolescents. It is more common in areas of Asia that have high rates of hepatitis B virus infection than in the U.S.
Hepatocellular carcinoma is the most common type of liver cancer in adults. Risk factors, staging, and treatment for children is different than for adults. For information about hepatocellular carcinoma in adults, see What Is Liver Cancer?.
Signs and symptoms of childhood hepatocellular carcinoma
Signs and symptoms are more common after the tumor gets big. Other conditions can cause the same signs and symptoms. Check with your child’s doctor if your child has any of the following:
- a lump in the abdomen that may be painful
- swelling in the abdomen
- weight loss for no known reason
- loss of appetite
- nausea and vomiting
Causes and risk factors for childhood hepatocellular carcinoma
Anything that increases your chance of getting a disease is called a risk factor. Not every child with one or more of these risk factors will develop hepatocellular carcinoma, and hepatocellular carcinoma will develop in some children who don’t have any known risk factors. Talk with your child’s doctor if you think your child may be at risk.
The following syndromes or conditions are risk factors for childhood hepatocellular carcinoma:
- Alagille syndrome.
- Glycogen storage disease.
- Hepatitis B virus infection that was passed from mother to child at birth.
- Progressive familial intrahepatic disease.
- Tyrosinemia: Some patients with tyrosinemia are diagnosed with hepatocellular carcinoma after receiving a liver transplant, before there are signs or symptoms of cancer.
Hepatocellular carcinoma may develop in children with no underlying liver disease.
Diagnosis of childhood hepatocellular carcinoma
Tests that examine the liver and the blood are used to diagnose childhood hepatocellular carcinoma and find out whether it has spread.
The following tests and procedures may be used:
- Physical exam and health history: A physical exam of the body will be done to check a person’s health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient's health habits and past illnesses and treatments will also be taken.
- Serum tumor marker test: This blood test measures the amounts of certain substances released into the blood by organs, tissues, or tumor cells in the body. Certain substances are linked to specific types of cancer when found in increased levels in the blood. These are called tumor markers. The blood of children who have liver cancer may have increased amounts of a hormone called beta-human chorionic gonadotropin (beta-hCG) or a protein called alpha-fetoprotein (AFP). Other cancers, benign liver tumors, and certain noncancer conditions, including cirrhosis and hepatitis, can also increase AFP levels.
-
Complete blood count (CBC): A sample of blood is drawn and checked for the following:
- the number of red blood cells, white blood cells, and platelets
- the amount of hemoglobin (the protein that carries oxygen) in the red blood cells
- the portion of the blood sample made up of red blood cells
- Liver function tests: These blood tests measure the amounts of certain substances released into the blood by the liver. A higher-than-normal amount of a substance can be a sign of liver damage or cancer.
- Blood chemistry studies: These blood tests measure the amounts of certain substances, such as bilirubin or lactate dehydrogenase (LDH), released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
- Epstein-Barr virus (EBV) test: This blood test checks for antibodies to the EBV and DNA markers of the EBV. These are found in the blood of patients who have been infected with EBV.
- Hepatitis assay: This blood test checks for pieces of the hepatitis virus.
-
Magnetic resonance imaging (MRI) with gadolinium: This procedure uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the liver. A substance called gadolinium is injected into a vein. The gadolinium collects around the cancer cells so they show up brighter in the picture.

Magnetic resonance imaging (MRI) scan. The child lies on a table that slides into the MRI machine, which takes a series of detailed pictures of areas inside the body. The positioning of the child on the table depends on the part of the body being imaged. -
CT scan (CAT scan): This procedure uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body, taken from different angles. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. In childhood liver cancer, a CT scan of the chest and abdomen is usually done.

Computed tomography (CT) scan. The child lies on a table that slides through the CT scanner, which takes a series of detailed x-ray pictures of areas inside the body. -
Ultrasound exam: This procedure uses high-energy sound waves (ultrasound) that are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. In childhood liver cancer, an ultrasound exam of the abdomen to check the large blood vessels is usually done.

Abdominal ultrasound. An ultrasound transducer connected to a computer is pressed against the skin of the abdomen. The transducer bounces sound waves off internal organs and tissues to make echoes that form a sonogram (computer picture). - Abdominal x-ray: An x-ray of the organs in the abdomen may be done. An x-ray is a type of energy beam that can go through the body onto film, making a picture of areas inside the body.
-
Biopsy: During a biopsy, a doctor removes a sample of cells or tissue. A pathologist then views the cells or tissue under a microscope to look for cancer cells and find out the type of cancer. The doctor may remove as much tumor as safely possible during the same biopsy procedure.
The following test may be done on the sample of tissue that is removed:
- Immunohistochemistry: This laboratory test uses antibodies to check for certain antigens (markers) in a sample of a patient’s tissue. The antibodies are usually linked to an enzyme or a fluorescent dye. After the antibodies bind to a specific antigen in the tissue sample, the enzyme or dye is activated, and the antigen can then be seen under a microscope. This type of test is used to check for a certain gene mutation, to help diagnose cancer, and to help tell one type of cancer from another type of cancer.
Prognostic factors for childhood hepatocellular carcinoma
The prognosis (chance of recovery) and treatment options for childhood hepatocellular carcinoma depend on the following:
- the PRETEXT group
- whether the cancer has spread to other places in the body, such as the lungs
- whether the cancer can be removed completely by surgery
- how the cancer responds to chemotherapy
- whether the child has hepatitis B virus infection
- whether the cancer has just been diagnosed or has recurred
For childhood hepatocellular carcinoma that recurs (comes back) after initial treatment, the prognosis and treatment options depend on the following:
- where in the body the tumor recurred
- the type of treatment used to treat the initial cancer
Childhood liver cancer may be cured if the tumor is small and can be completely removed by surgery. Complete removal is possible more often for hepatoblastoma than for hepatocellular carcinoma.
Stages of childhood hepatocellular carcinoma
After childhood hepatocellular carcinoma has been diagnosed, tests are done to find out if cancer cells have spread within the liver or to other parts of the body. The process used to find out if cancer has spread within the liver, to nearby tissues or organs, or to other parts of the body is called staging. In childhood hepatocellular carcinoma, the PRETEXT and POSTTEXT groups are used instead of stage to plan treatment. The results of the tests and procedures done to detect, diagnose, and find out whether the cancer has spread are used to determine the PRETEXT and POSTTEXT groups.
Two grouping systems are used for childhood hepatocellular carcinoma to decide whether the tumor can be removed by surgery:
- The PRETEXT group describes the tumor the patient has any treatment.
- The POSTTEXT group describes the tumor the patient has had treatment such as neoadjuvant chemotherapy.
The liver is divided into four sections. The PRETEXT and POSTTEXT groups depend on which sections of the liver have cancer.
PRETEXT and POSTTEXT group I

Liver PRETEXT and POSTTEXT I. Cancer is found in one section of the liver. Three sections of the liver that are next to each other do not have cancer in them. In group I, the cancer is found in one section of the liver. Three sections of the liver that are next to each other do not have cancer in them.
PRETEXT and POSTTEXT group II

Liver PRETEXT and POSTTEXT II. Cancer is found in one or two sections of the liver. Two sections of the liver that are next to each other do not have cancer in them. In group II, cancer is found in one or two sections of the liver. Two sections of the liver that are next to each other do not have cancer in them.
PRETEXT and POSTTEXT group III

Liver PRETEXT and POSTTEXT III. Cancer is found in three sections of the liver and one section does not have cancer in it, or cancer is found in two sections of the liver and two sections that are not next to each other do not have cancer in them. In group III, one of the following is true:
- Cancer is found in three sections of the liver and one section does not have cancer.
- Cancer is found in two sections of the liver and two sections that are not next to each other do not have cancer in them.
PRETEXT and POSTTEXT group IV

Liver PRETEXT and POSTTEXT IV. Cancer is found in all four sections of the liver. In group IV, cancer is found in all four sections of the liver.
Sometimes childhood hepatocellular carcinoma continues to grow or comes back after treatment.
Progressive disease is cancer that continues to grow, spread, or worsen. Progressive disease may be a sign that the cancer has become refractory to treatment.
Recurrent childhood hepatocellular carcinoma is cancer that has recurred (come back) after it has been treated. The cancer may come back in the liver or in other parts of the body. To learn more about metastatic cancer (cancer that has spread from where it started to other parts of the body), see Metastatic Cancer: When Cancer Spreads.
Types of treatment for childhood hepatocellular carcinoma
Children with hepatocellular carcinoma should have their treatment planned by a team of healthcare providers who are experts in treating this rare childhood cancer. Treatment will be overseen by a pediatric oncologist, a doctor who specializes in treating children with cancer. The pediatric oncologist works with other healthcare providers who are experts in treating children with hepatocellular carcinoma and who specialize in certain areas of medicine. It is especially important to have a pediatric surgeon with experience in liver surgery who can send patients to a liver transplant program if needed. Other specialists may include the following:
- pediatrician
- radiation oncologist
- pediatric nurse specialist
- rehabilitation specialist
- psychologist
- social worker
- nutritionist
For more information about having a child with cancer and ways to cope and find support, see Childhood Cancers.
Every child will not receive all the treatments listed below. Your child’s care team will help you make treatment decisions based on your child’s unique situation. To learn more about factors that help determine the treatment plan for childhood hepatocellular carcinoma, see Prognostic factors for childhood hepatocellular carcinoma.
Surgery
When possible, the cancer is removed by surgery. The types of surgery that may be done are:
- Partial hepatectomy: The part of the liver where cancer is found is removed by surgery. The part removed may be a wedge of tissue, an entire lobe, or a larger part of the liver, along with a small amount of normal tissue around it.
- Total hepatectomy and liver transplant: The entire liver is removed by surgery, followed by a transplant of a healthy liver from a donor. A liver transplant may be possible when cancer has not spread beyond the liver and a donated liver can be found. If the patient has to wait for a donated liver, other treatment is given as needed.
- Resection of metastases: Surgery is done to remove cancer that has spread outside of the liver, such as to nearby tissues, the lungs, or the brain.
The type of surgery that can be done depends on the following:
- the PRETEXT group and POSTTEXT group
- the size of the primary tumor
- whether there is more than one tumor in the liver
- whether the cancer has spread to nearby large blood vessels
- the level of AFP in the blood
- whether the tumor can be shrunk by chemotherapy so that it can be removed by surgery
- whether a liver transplant is needed
Chemotherapy is sometimes given before surgery to shrink the tumor and make it easier to remove. This is called neoadjuvant therapy.
After the doctor removes all the cancer that can be seen at the time of the surgery, some patients may be given chemotherapy or radiation therapy after surgery to kill any cancer cells that are left. Treatment given after the surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy). Treatment using more than one anticancer drug is called combination chemotherapy.
Chemoembolization of the hepatic artery (the main artery that supplies blood to the liver) is a type of regional chemotherapy used to treat childhood liver cancer that cannot be removed by surgery. The anticancer drug is injected into the hepatic artery through a catheter (thin tube). The drug is mixed with a substance that blocks the artery, cutting off blood flow to the tumor. Most of the anticancer drug is trapped near the tumor and only a small amount of the drug reaches other parts of the body. The blockage may be temporary or permanent, depending on the substance used to block the artery. The tumor is prevented from getting the oxygen and nutrients it needs to grow. The liver continues to receive blood from the hepatic portal vein, which carries blood from the stomach and intestine to the liver. This procedure is also called transarterial chemoembolization or TACE.
The way the chemotherapy is given depends on the type of the cancer being treated and the PRETEXT or POSTTEXT group.
To learn more about chemotherapy and its side effects, see Chemotherapy and You: Support for People with Cancer.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
- Radioembolization is a type of internal radiation therapy used to treat hepatocellular carcinoma. A very small amount of a radioactive substance is attached to tiny beads that are injected into the hepatic artery (the main artery that supplies blood to the liver) through a thin tube called a catheter. The beads are mixed with a substance that blocks the artery, cutting off blood flow to the tumor. Most of the radiation is trapped near the tumor to kill the cancer cells. This is done to relieve symptoms and improve quality of life for children with hepatocellular carcinoma.
To learn more about radiation therapy and its side effects, see Radiation Therapy to Treat Cancer and Radiation Therapy Side Effects.
Antiviral treatment
Hepatocellular carcinoma that is linked to the hepatitis B virus may be treated with antiviral drugs.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells. Targeted therapies usually cause less harm to normal cells than chemotherapy or radiation therapy do. Targeted therapy is being studied for the treatment of hepatocellular carcinoma that has come back after treatment.
To learn more about how targeted therapy works against cancer, what to expect when having targeted therapy, and targeted therapy side effects, see Targeted Therapy to Treat Cancer.
Clinical trials
A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. For some patients, taking part in a clinical trial may be an option.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
To learn more about clinical trials, see Clinical Trials Information for Patients and Caregivers.
Long-term side effects of treatment
Side effects from cancer treatment that begin after treatment and continue for months or years are called long-term or late effects. Late effects of cancer treatment may include the following:
- physical problems
- changes in mood, feelings, thinking, learning, or memory
- second cancers (new types of cancer)
Some late effects may be treated or controlled. It is important to talk with your child's doctors about the long-term effects cancer treatment can have on your child. For more information, see Late Effects of Treatment for Childhood Cancer.
Follow-up tests
Some of the tests that were done to diagnose the cancer or to find out the treatment group may be repeated. Some tests will be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Treatment of newly diagnosed childhood hepatocellular carcinoma
Treatment options for newly diagnosed hepatocellular carcinoma that can be removed by surgery at the time of diagnosis may include the following:
- surgery alone to remove the tumor
- surgery to remove the tumor, followed by chemotherapy with cisplatin and doxorubicin
- combination chemotherapy, followed by surgery to remove the tumor
Treatment options for newly diagnosed hepatocellular carcinoma that cannot be removed by surgery and has not spread to other parts of the body at the time of diagnosis may include the following:
- chemotherapy to shrink the tumor, followed by surgery to completely remove the tumor
- chemotherapy to shrink the tumor
If surgery to completely remove the tumor is not possible, further treatment may include the following:
- liver transplant
- chemoembolization of the hepatic artery to shrink the tumor, followed by surgery to remove the tumor or liver transplant
- chemoembolization of the hepatic artery alone
- chemoembolization followed by liver transplant
- radioembolization of the hepatic artery as palliative therapy to relieve symptoms and improve the quality of life
Treatment for newly diagnosed hepatocellular carcinoma that has spread to other parts of the body at the time of diagnosis may include the following:
- Combination chemotherapy to shrink the tumor, followed by surgery to remove as much of the tumor as possible from the liver and other places where cancer has spread. Studies have not shown that this treatment works well but some patients may have some benefit.
Treatment options for newly diagnosed hepatocellular carcinoma related to hepatitis B virus (HBV) infection may include the following:
- surgery to remove the tumor
- antiviral drugs that treat infection caused by the hepatitis B virus
Treatment options in clinical trials for newly diagnosed hepatocellular carcinoma may include the following:
- a clinical trial of chemotherapy and surgery
Treatment of progressive or recurrent childhood hepatocellular carcinoma
Treatment of progressive or recurrent hepatocellular carcinoma may include the following:
- chemoembolization of the hepatic artery to shrink the tumor before liver transplant
- liver transplant
- a clinical trial of targeted therapy (sorafenib or pazopanib)
- a clinical trial that checks a sample of the patient's tumor for certain gene changes to determine the type of targeted therapy that will be given
- Childhood Undifferentiated Embryonal Sarcoma of the Liver
-
Childhood undifferentiated embryonal sarcoma of the liver is a rare cancer type that forms in the tissues of the liver. This type of liver cancer usually occurs in children between 5 and 10 years. It often spreads all through the liver and/or to the lungs.
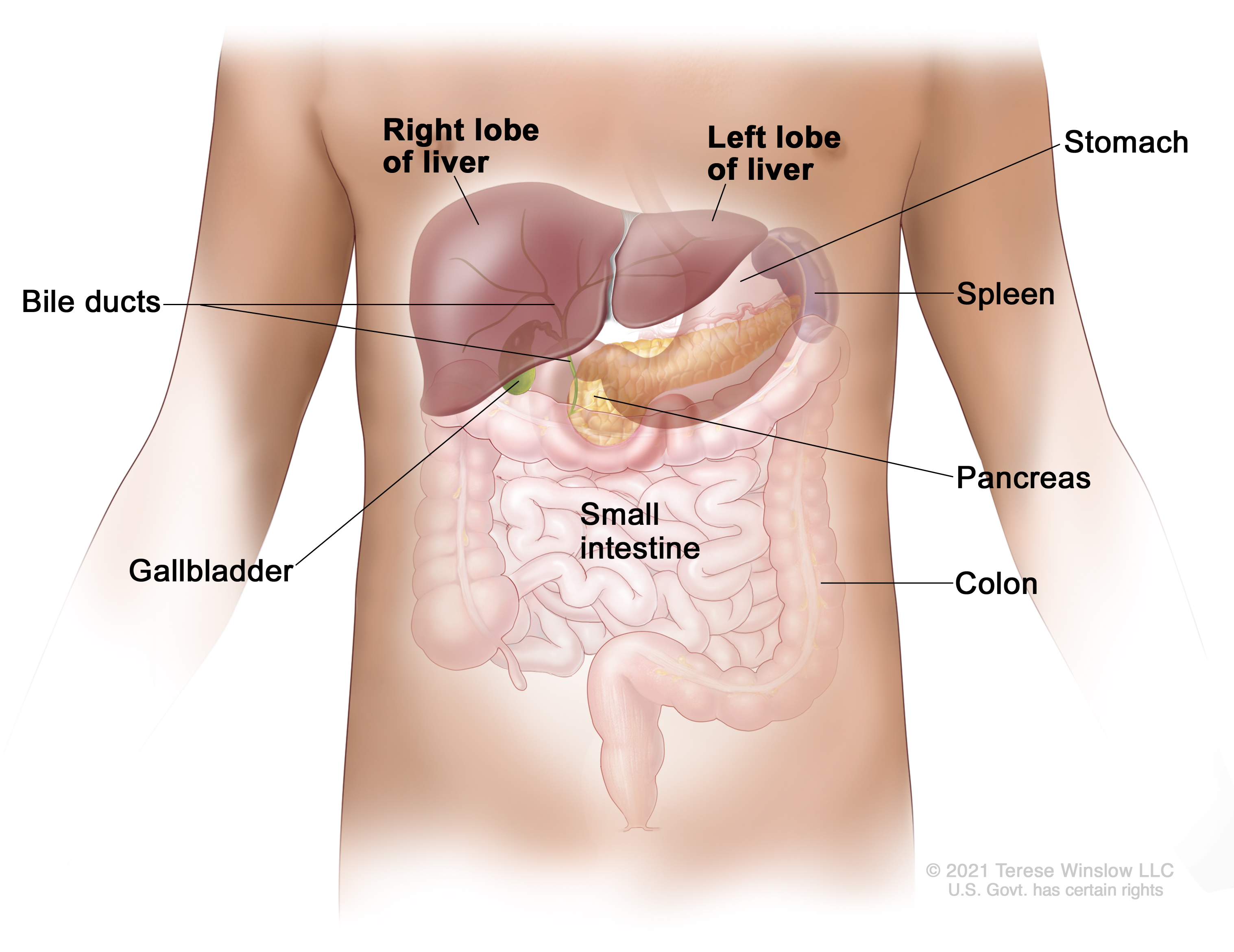
The liver is one of the largest organs in the body. It has two lobes and fills the upper right side of the abdomen inside the rib cage. Three of the many important functions of the liver are the following:
- to make bile to help digest fats from food
- to store glycogen (sugar), which the body uses for energy
- to filter harmful substances from the blood so they can be passed from the body in stools and urine
Anatomy of the liver. The liver is in the upper abdomen near the stomach, intestines, gallbladder, and pancreas. The liver has a right lobe and a left lobe. Each lobe is divided into two sections (not shown). Signs and symptoms of childhood undifferentiated embryonal sarcoma of the liver
Signs and symptoms are more common after the tumor gets big. These and other signs and symptoms may be caused by undifferentiated embryonal sarcoma of the liver or by other conditions. Check with your child’s doctor if your child has any of the following:
- a lump in the abdomen that may be painful
- swelling in the abdomen
Diagnosis of childhood undifferentiated embryonal sarcoma of the liver
Tests that examine the liver and the blood are used to diagnose childhood undifferentiated embryonal sarcoma of the liver and find out whether the cancer has spread.
The following tests and procedures may be used:
- Physical exam and health history: A physical exam of the body will be done to check a person’s health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient's health habits and past illnesses and treatments will also be taken.
-
Complete blood count (CBC): A sample of blood is drawn and checked for the following:
- the number of red blood cells, white blood cells, and platelets
- the amount of hemoglobin (the protein that carries oxygen) in the red blood cells
- the portion of the blood sample made up of red blood cells
- Liver function tests: These blood tests measure the amounts of certain substances released into the blood by the liver. A higher-than-normal amount of a substance can be a sign of liver damage or cancer.
- Blood chemistry studies: These blood tests measure the amounts of certain substances, such as bilirubin or lactate dehydrogenase (LDH), released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
-
Magnetic resonance imaging (MRI) with gadolinium: This procedure uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the liver. A substance called gadolinium is injected into a vein. The gadolinium collects around the cancer cells so they show up brighter in the picture.

Magnetic resonance imaging (MRI) scan. The child lies on a table that slides into the MRI machine, which takes a series of detailed pictures of areas inside the body. The positioning of the child on the table depends on the part of the body being imaged. -
CT scan (CAT scan): This procedure uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body, taken from different angles. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. In childhood liver cancer, a CT scan of the chest and abdomen is usually done.

Computed tomography (CT) scan. The child lies on a table that slides through the CT scanner, which takes a series of detailed x-ray pictures of areas inside the body. -
Ultrasound exam: This procedure uses high-energy sound waves (ultrasound) that are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. In childhood liver cancer, an ultrasound exam of the abdomen to check the large blood vessels is usually done.

Abdominal ultrasound. An ultrasound transducer connected to a computer is pressed against the skin of the abdomen. The transducer bounces sound waves off internal organs and tissues to make echoes that form a sonogram (computer picture). - Abdominal x-ray: An x-ray of the organs in the abdomen may be done. An x-ray is a type of energy beam that can go through the body onto film, making a picture of areas inside the body.
-
Biopsy: During a biopsy, a doctor removes a sample of cells or tissue. A pathologist then views the cells or tissue under a microscope to look for cancer cells and find out the type of cancer. The doctor may remove as much tumor as safely possible during the same biopsy procedure.
The following test may be done on the sample of tissue that is removed:
- Immunohistochemistry: This laboratory test uses antibodies to check for certain antigens (markers) in a sample of a patient’s tissue. The antibodies are usually linked to an enzyme or a fluorescent dye. After the antibodies bind to a specific antigen in the tissue sample, the enzyme or dye is activated, and the antigen can then be seen under a microscope. This type of test is used to check for a certain gene mutation, to help diagnose cancer, and to help tell one type of cancer from another type of cancer.
Prognostic factors for childhood undifferentiated embryonal sarcoma of the liver
The prognosis (chance of recovery) and treatment options depend on the following:
- the size of the tumor
- the health of the patient
- how the cancer responds to chemotherapy
- whether the cancer can be removed completely by surgery
- whether the patient can have a liver transplant
- whether the cancer has just been diagnosed or has recurred
For childhood undifferentiated embryonal sarcoma of the liver that recurs (comes back) after initial treatment, the prognosis and treatment options depend on the following:
- where in the body the tumor recurred
- the type of treatment used to treat the initial cancer
Types of treatment for childhood undifferentiated embryonal sarcoma of the liver
Children with undifferentiated embryonal sarcoma of the liver should have their treatment planned by a team of healthcare providers who are experts in treating this rare childhood cancer. Treatment will be overseen by a pediatric oncologist, a doctor who specializes in treating children with cancer. The pediatric oncologist works with other healthcare providers who are experts in treating children with undifferentiated embryonal sarcoma of the liver and who specialize in certain areas of medicine. It is especially important to have a pediatric surgeon with experience in liver surgery who can send patients to a liver transplant program if needed. Other specialists may include the following:
- pediatrician
- radiation oncologist
- pediatric nurse specialist
- rehabilitation specialist
- psychologist
- social worker
- nutritionist
For more information about having a child with cancer and ways to cope and find support, see Childhood Cancers.
Every child will not receive all the treatments listed below. Your child’s care team will help you make treatment decisions based on your child’s unique situation. To learn more about factors that help determine the treatment plan for this cancer, see Prognostic factors for childhood undifferentiated embryonal sarcoma of the liver.
Surgery
A partial hepatectomy (surgery to remove the part of the liver where cancer is found) may be done. A wedge of tissue, an entire lobe, or a larger part of the liver, along with some of the healthy tissue around it is removed. The remaining liver tissue takes over the functions of the liver and may regrow.
Liver transplant
In a liver transplant, the entire liver is removed by surgery and replaced with a healthy donated liver. A liver transplant may be done when the cancer is in the liver only and a donated liver can be found. If the patient has to wait for a donated liver, other treatment is given as needed.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). Treatment using more than one anticancer drug is called combination chemotherapy.
To learn more about chemotherapy and its side effects, see Chemotherapy and You: Support for People with Cancer.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells. Targeted therapies usually cause less harm to normal cells than chemotherapy or radiation therapy do. Targeted therapy is being studied for the treatment of undifferentiated embryonal sarcoma of the liver that has come back after treatment.
To learn more about how targeted therapy works against cancer, what to expect when having targeted therapy, and targeted therapy side effects, see Targeted Therapy to Treat Cancer.
Clinical trials
A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. For some patients, taking part in a clinical trial may be an option.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
To learn more about clinical trials, see Clinical Trials Information for Patients and Caregivers.
Long-term side effects of treatment
Side effects from cancer treatment that begin after treatment and continue for months or years are called long-term or late effects. Late effects of cancer treatment may include the following:
- physical problems
- changes in mood, feelings, thinking, learning, or memory
- second cancers (new types of cancer)
Some late effects may be treated or controlled. It is important to talk with your child's doctors about the long-term effects cancer treatment can have on your child. For more information, see Late Effects of Treatment for Childhood Cancer.
Follow-up tests
Some of the tests that were done to diagnose the cancer or to find out the treatment group may be repeated. Some tests will be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Treatment of newly diagnosed childhood undifferentiated embryonal sarcoma of the liver
Treatment of newly diagnosed childhood undifferentiated embryonal sarcoma of the liver may include the following:
- Combination chemotherapy may be used to shrink the tumor, followed by surgery to remove as much of the tumor as possible. Chemotherapy may also be given after surgery to remove the tumor.
- Surgery may be done to remove the tumor, followed by chemotherapy. A second surgery may be done to remove tumor that remains, followed by more chemotherapy.
- Liver transplant may be done if surgery to remove the tumor is not possible.
Treatment of progressive or recurrent childhood undifferentiated embryonal sarcoma of the liver
Sometimes childhood undifferentiated embryonal sarcoma of the liver continues to grow or comes back after treatment.
- Progressive disease is cancer that continues to grow, spread, or worsen. Progressive disease may be a sign that the cancer has become refractory to treatment.
- Recurrent childhood undifferentiated embryonal sarcoma of the liver is cancer that has recurred (come back) after it has been treated. The cancer may come back in the liver or in other parts of the body.
To learn more about metastatic cancer (cancer that has spread from where it started to other parts of the body), see Metastatic Cancer: When Cancer Spreads.
Treatment of recurrent childhood undifferentiated embryonal sarcoma of the liver may include the following:
- a clinical trial that checks a sample of the patient's tumor for certain gene changes to determine the type of targeted therapy that will be given
- Infantile Choriocarcinoma of the Liver
-
Infantile choriocarcinoma of the liver is a very rare type of cancer that starts in the placenta and spreads to the fetus. The tumor is usually found during the first few months after the baby is born.
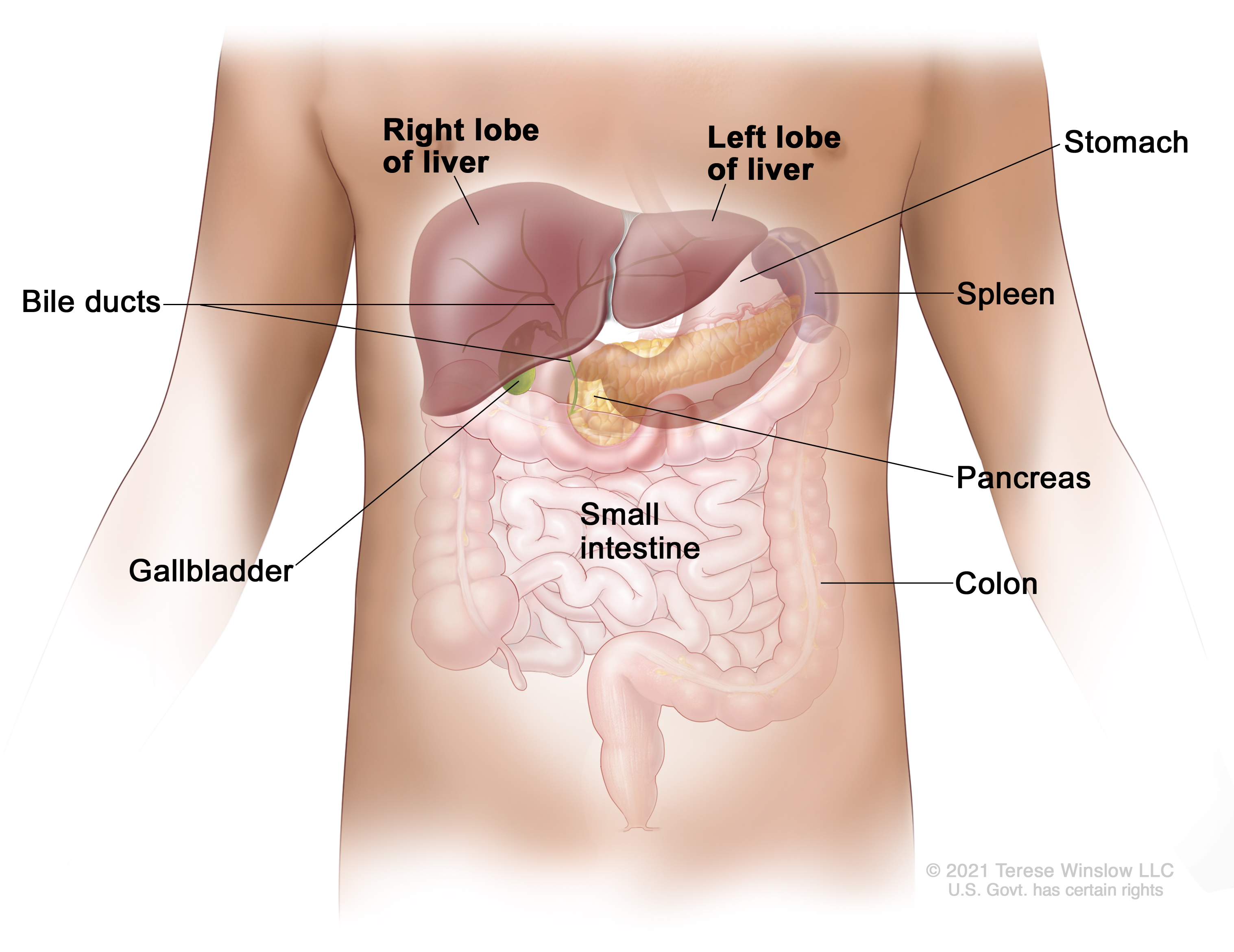
The liver is one of the largest organs in the body. It has two lobes and fills the upper right side of the abdomen inside the rib cage. Three of the many important functions of the liver are the following:
- to make bile to help digest fats from food
- to store glycogen (sugar), which the body uses for energy
- to filter harmful substances from the blood so they can be passed from the body in stools and urine
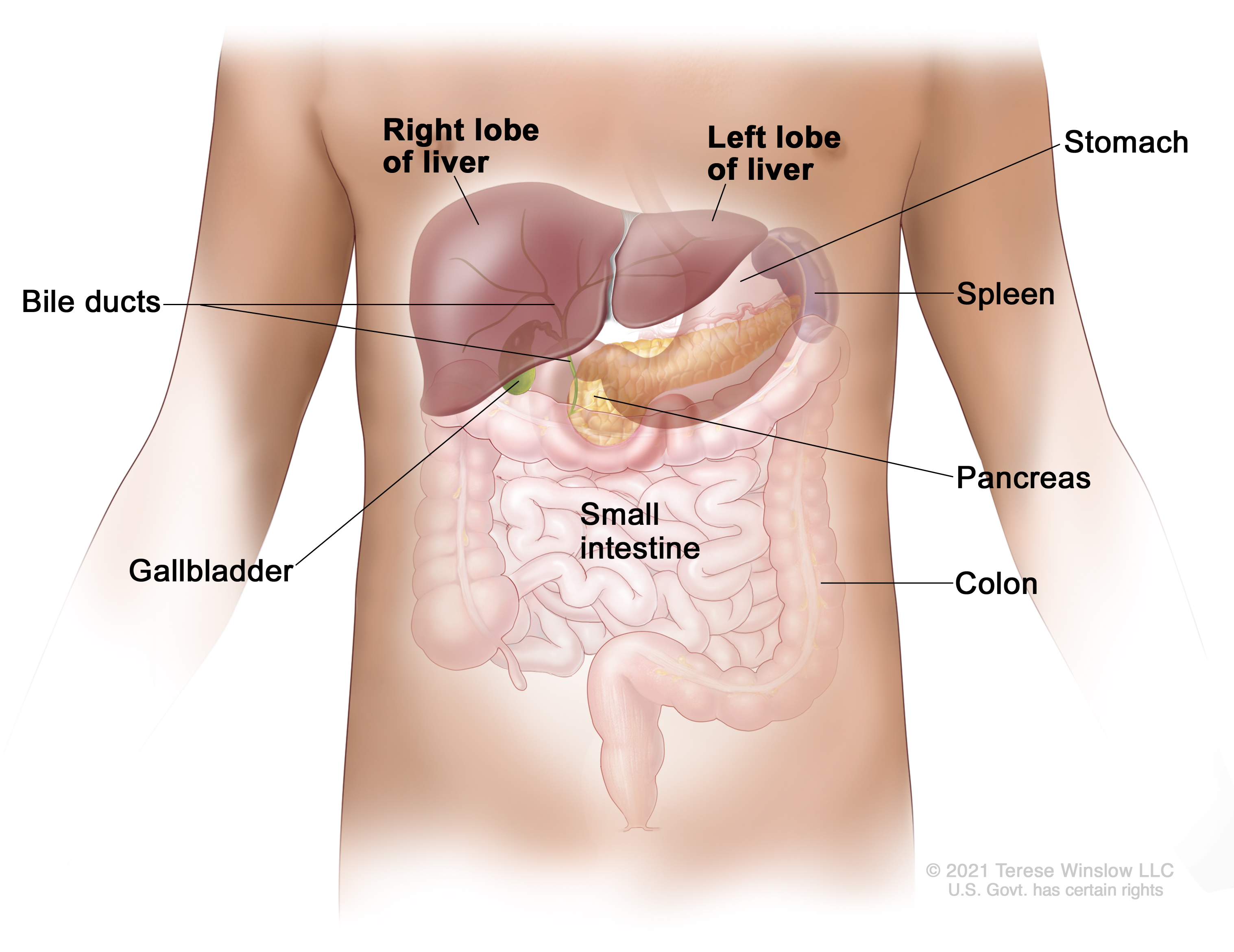
Anatomy of the liver. The liver is in the upper abdomen near the stomach, intestines, gallbladder, and pancreas. The liver has a right lobe and a left lobe. Each lobe is divided into two sections (not shown). The mother of the child may also be diagnosed with choriocarcinoma. See Gestational Trophoblastic Disease Treatment for more information on the treatment of choriocarcinoma for the mother.
Signs and symptoms of infantile choriocarcinoma of the liver
Signs and symptoms are more common after the tumor gets big. These and other signs and symptoms may be caused by infantile choriocarcinoma or by other conditions. Check with your child’s doctor if your child has any of the following:
- a lump in the abdomen
- swelling in the abdomen
- hemorrhage
Diagnosis of infantile choriocarcinoma of the liver
Tests that examine the liver and the blood are used to diagnose infantile choriocarcinoma of the liver and find out whether the cancer has spread. The following tests and procedures may be used:
- Physical exam and health history: A physical exam of the body will be done to check a person’s health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient's health habits and past illnesses and treatments will also be taken.
- Serum tumor marker test: This blood test measures the amounts of certain substances released into the blood by organs, tissues, or tumor cells in the body. Certain substances are linked to specific types of cancer when found in increased levels in the blood. These are called tumor markers. The blood of children who have liver cancer may have increased amounts of a hormone called beta-human chorionic gonadotropin (beta-hCG) or a protein called alpha-fetoprotein (AFP). Other cancers, benign liver tumors, and certain noncancer conditions, including cirrhosis and hepatitis, can also increase AFP levels.
-
Complete blood count (CBC): A sample of blood is drawn and checked for the following:
- the number of red blood cells, white blood cells, and platelets
- the amount of hemoglobin (the protein that carries oxygen) in the red blood cells
- the portion of the blood sample made up of red blood cells
- Liver function tests: These blood tests measure the amounts of certain substances released into the blood by the liver. A higher-than-normal amount of a substance can be a sign of liver damage or cancer.
- Blood chemistry studies: These blood tests measure the amounts of certain substances, such as bilirubin or lactate dehydrogenase (LDH), released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
-
Magnetic resonance imaging (MRI) with gadolinium: This procedure uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the liver. A substance called gadolinium is injected into a vein. The gadolinium collects around the cancer cells so they show up brighter in the picture.

Magnetic resonance imaging (MRI) scan. The child lies on a table that slides into the MRI machine, which takes a series of detailed pictures of areas inside the body. The positioning of the child on the table depends on the part of the body being imaged. -
CT scan (CAT scan): This procedure uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body, taken from different angles. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. In childhood liver cancer, a CT scan of the chest and abdomen is usually done.

Computed tomography (CT) scan. The child lies on a table that slides through the CT scanner, which takes a series of detailed x-ray pictures of areas inside the body. -
Ultrasound exam: This procedure uses high-energy sound waves (ultrasound) that are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. In childhood liver cancer, an ultrasound exam of the abdomen to check the large blood vessels is usually done.

Abdominal ultrasound. An ultrasound transducer connected to a computer is pressed against the skin of the abdomen. The transducer bounces sound waves off internal organs and tissues to make echoes that form a sonogram (computer picture). - Abdominal x-ray: An x-ray of the organs in the abdomen may be done. An x-ray is a type of energy beam that can go through the body onto film, making a picture of areas inside the body.
-
Biopsy: During a biopsy, a doctor removes a sample of cells or tissue. A pathologist then views the cells or tissue under a microscope to look for cancer cells and find out the type of cancer. If cancer cells are found, the doctor may remove as much tumor as safely possible during the same biopsy procedure.
The following test may be done on the sample of tissue that is removed:
- Immunohistochemistry: This laboratory test uses antibodies to check for certain antigens (markers) in a sample of a patient’s tissue. The antibodies are usually linked to an enzyme or a fluorescent dye. After the antibodies bind to a specific antigen in the tissue sample, the enzyme or dye is activated, and the antigen can then be seen under a microscope. This type of test is used to check for a certain gene mutation, to help diagnose cancer, and to help tell one type of cancer from another type of cancer.
Prognostic factors for infantile choriocarcinoma of the liver
The prognosis (chance of recovery) and treatment options for infantile choriocarcinoma of the liver depend on the following:
- the size of the tumor
- the health of the patient
- how the cancer responds to chemotherapy
- whether the cancer can be removed completely by surgery
- whether the patient can have a liver transplant
- whether the cancer has just been diagnosed or has recurred
For infantile choriocarcinoma of the liver that recurs (comes back) after initial treatment, the prognosis and treatment options depend on the following:
- where in the body the tumor recurred
- the type of treatment used to treat the initial cancer
Types of treatment for infantile choriocarcinoma of the liver
Children with infantile choriocarcinoma of the liver should have their treatment planned by a team of healthcare providers who are experts in treating this rare childhood cancer. Treatment will be overseen by a pediatric oncologist, a doctor who specializes in treating children with cancer. The pediatric oncologist works with other healthcare providers who are experts in treating children with infantile choriocarcinoma of the liver and who specialize in certain areas of medicine. It is especially important to have a pediatric surgeon with experience in liver surgery who can send patients to a liver transplant program if needed. Other specialists may include the following:
- pediatrician
- radiation oncologist
- pediatric nurse specialist
- rehabilitation specialist
- psychologist
- social worker
- nutritionist
For more information about having a child with cancer and ways to cope and find support, see Childhood Cancers.
Every child will not receive all the treatments listed below. Your child’s care team will help you make treatment decisions based on your child’s unique situation. To learn more about factors that help determine the treatment plan for this cancer, see Prognostic factors for infantile choriocarcinoma of the liver.
Surgery
A partial hepatectomy (surgery to remove the part of the liver where cancer is found) may be done. A wedge of tissue, an entire lobe, or a larger part of the liver, along with some of the healthy tissue around it is removed. The remaining liver tissue takes over the functions of the liver and may regrow.
Liver transplant
In a liver transplant, the entire liver is removed by surgery and replaced with a healthy donated liver. A liver transplant may be done when the cancer is in the liver only and a donated liver can be found. If the patient has to wait for a donated liver, other treatment is given as needed.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). Treatment using more than one anticancer drug is called combination chemotherapy. To learn more about chemotherapy and its side effects, see Chemotherapy and You: Support for People with Cancer.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells. Targeted therapies usually cause less harm to normal cells than chemotherapy or radiation therapy do. Targeted therapy is being studied for the treatment of infantile choriocarcinoma of the liver that has come back after treatment.
To learn more about how targeted therapy works against cancer, what to expect when having targeted therapy, and targeted therapy side effects, see Targeted Therapy to Treat Cancer.
Clinical trials
A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. For some patients, taking part in a clinical trial may be an option.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
To learn more about clinical trials, see Clinical Trials Information for Patients and Caregivers.
Long-term side effects of treatment
Side effects from cancer treatment that begin after treatment and continue for months or years are called long-term or late effects. Late effects of cancer treatment may include the following:
- physical problems
- changes in mood, feelings, thinking, learning, or memory
- second cancers (new types of cancer)
Some late effects may be treated or controlled. It is important to talk with your child's doctors about the long-term effects cancer treatment can have on your child. For more information, see Late Effects of Treatment for Childhood Cancer.
Follow-up tests
Some of the tests that were done to diagnose the cancer or to find out the treatment group may be repeated. Some tests will be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Treatment of newly diagnosed infantile choriocarcinoma of the liver
Treatment of newly diagnosed infantile choriocarcinoma of the liver may include the following:
- surgery to remove the tumor
- combination chemotherapy to shrink the tumor, followed by surgery to remove the tumor
- chemotherapy to treat the tumor followed by liver transplant
Treatment of progressive or recurrent infantile choriocarcinoma of the liver
Sometimes infantile choriocarcinoma of the liver continues to grow or comes back after treatment.
- Progressive disease is cancer that continues to grow, spread, or worsen. Progressive disease may be a sign that the cancer has become refractory to treatment.
- Recurrent infantile choriocarcinoma of the liver is cancer that has recurred (come back) after it has been treated. The cancer may come back in the liver or in other parts of the body.
To learn more about metastatic cancer (cancer that has spread from where it started to other parts of the body), see Metastatic Cancer: When Cancer Spreads.
Treatment of progressive or recurrent infantile choriocarcinoma of the liver may include the following:
- a clinical trial that checks a sample of the patient's tumor for certain gene changes to determine the type of targeted therapy that will be given

 画像を拡大する
画像を拡大する